We're exploring the concepts of holistic nutrition and bioindividuality. I discuss the various nutrition professionals and their titles, and how varying nutrition paradigms and views exist. Lastly, we'll cover the beginning steps that you can take to start your journey using holistic nutrition to support you and your family's health and wellness. Enjoy!
How My Chronic Illness Was a Catalyst to a Career Change...The Story of ‘Speaking of’ (Part 2)
Episode 2 of the podcast is Part 2 of a two part story about how my chronic illness was a catalyst to career change, and how Speaking of Health & Wellness came to be! Be sure to listen to Part 1 first or you may be a bit lost... I shared my personal experience with medical injury and chronic illness.
We're starting where we left off: with my experience with the "Mirena crash" and my path into true holistic healing, which ultimately led me to understanding autism spectrum disorders (and more) as whole body conditions and changed the trajectory of my career.
How My Chronic Illness Was a Catalyst to a Career Change...The Story of ‘Speaking of’ (Part 1)
On this first episode of Speaking of Health & Wellness: The Podcast…
I’m introducing myself and my intentions with this podcast, as well as sharing the story of how my own health and wellness journey was the catalyst to becoming a holistic nutrition and development coach for parents of children with complex picky eating, developmental delays, and neurodevelopmental disorders. I share my personal experience with medical injury and chronic illness, and how it ultimately led me to understanding autism spectrum disorders (and more) as whole body conditions.
5 Holiday Meal Tips for Parents of Picky Eaters
For families navigating complex picky eating and/or special diets with their children, the holiday gatherings can be especially tricky.
Here are some simple and practical tips to help you navigate your child’s picky eating during holidays:
1. As I encourage you to do on a day-to-day basis, focus on positive food exposures and interactions without any expectations that they actually eat the food. At the holiday gathering and before!
As the holiday approaches, aim to give them some pre-exposure to these foods in the weeks leading up to the holiday at home. This doesn’t have to just be at mealtimes!
There are so many ways you can thoughtfully add food exposures without expectation to eat. Here are a few ideas:
Ask them to help you pick out certain produce at the grocery store. Teaching them how to know when it’s ripe. Naming produce. Counting. Smelling. Talking about colors and touching the textures. This will obviously add time to your grocery store trip but perhaps we could reframe it. Think of it like a food exploration field trip!
Will they be hands-on with it outside of a meal at home, like with a craft or activity? EX: berries as paint, potatoes as stamps, broccoli or asparagus as a paint brush, etc.
Talk about the foods that are traditionally prepared at holidays, your own favorites, the foods they already like that will be there, the food colors, textures, shapes, smells, flavors, etc. Relate these foods to the ones they are already familiar with. EX: “sweet potatoes are orange, they feel like mashed potatoes in your mouth but they’re sweeter”.
Books are another great way to incorporate learning about foods without expectation that they eat the food! The day before, the day of, and on the way to the holiday gathering are ideal times for these conversations and books.
For especially complex picky eaters, a week or two ahead, starting to talk about the upcoming holiday meal might be even more helpful to decrease overwhelm. It may seem like you’re being really repetitive (you are) but if you’re child is struggling with complex picky eating, my guess is that they’ll find the repetition comforting as it’s letting them know what to expect.
2. Consider serving your child a meal before leaving for the holiday gathering.
I know, I know, you're probably thinking, "But they won't eat at the holiday gathering if they ate before we left". With children who are complex picky eaters, chances are that they won't be eating much at the holiday meal anyways, right?
Let’s be real. All of that unfamiliar food, a different environment, more people around, etc. So, to hopefully avoid any behaviors that may come up at the gathering due to hunger and blood sugar regulation, I suggest feeding your child a balanced meal at home before heading to the holiday gathering. Up the protein for longer satiation!
This will hopefully put less pressure on both of you around mealtimes while there, because you know they at least at a decent meal before leaving the house.
3. Bringing a dish? Choose something that you know they will eat. This way, you know there's at least one thing that your child prefers and can be successful with.
If your child is on a special diet or restricted because of food allergies/sensitivities/intolerances, check out my Recipe Inspiration page, where I’ve compiled my favorite recipe developers and cookbooks that feature whole food focused, gut-friendly, gluten-free recipes (often dairy free, allergy-friendly, and can easily be modified).
Get your kid involved in meal prepping the dish prior to the gathering (picking the produce out at the store, chopping, dicing, scooping, dumping, mixing, stirring, pressing a button, scraping into the bowl/pan/etc.).
If they’re capable, let them carry it to and/or hold it in the car. When you arrive, you can have your child share about what they've made with the host or other guests.
If they don't immediately run off to play when you arrive, walk the dish to the food table together and check out what else is there. Talk about what each dish is, who made it, how much love they put into the food, and what you're most looking forward to personally.
Reminder though: we are only looking for positive exposures to the foods. We are not expecting them to eat them. I repeat, we are NOT expecting that they eat these foods!
"Oh look there's Grandma's pumpkin pie that she makes every year. I can't wait to have some!"
"Wow, look at the sweet potato casserole. It's orange and it smells really sweet!"
4. Give them a "heads up" that the meal is coming.
Think of this from your child's point of view! Please do not just make your child's plate, interrupt them while they’re playing and having a blast with their cousins who they rarely see, and then expect them to come willingly sit and happily gobble up the plate of foods that aren't routinely familiar to them. I can't imagine that it'd go that well!
Instead, as you see mealtime is quickly approaching, give your child the heads up that in 3 minutes (or 5 minutes, 10 minutes, whatever your child needs) it's time to start getting their plate ready.
5. When it's time to eat, have them (or help them) make their own plate! Depending on their age and skill level, support them getting the food themselves.
You know they'll at least eat what you brought as a passing dish. What other foods are present that they may have prior exposure to? Did they show interest in any other foods when you were talking about them prior to this meal? Any foods that you think they'll probably (hopefully) try? Go for those first and in that order.
Keep any and all brand new food amounts small and underwhelming (like a dime, nickel, or quarter size - depending on the child and the food, of course), but aim for some variety on the plate. “Variety drives volume” one of my favorite SLP mentors ingrained in me.
For completely new foods, I would not push for more than 3 types of new foods during this time. We must remember, food and mealtimes are often overwhelming for these kids as it is at home…then when we add all the new variables of a holiday gathering, whoa! It can be very overwhelming to them!
Keep the opportunity for feelings of success present by not overloading or overwhelming the plate with too many new foods during holiday gatherings.
BONUS Tip…and perhaps most important to remember! :
Holidays are very food focused. For children who struggle with mealtimes (and their parents), this can add extra unnecessary anxiety to what should be a joyous occasion!
What if you gave yourself permission to let go of any focus or worry over what they will and won't eat, what they did or didn't eat? Go ahead. Let it go!
Have grace with yourself. With your child. With the entire process of introducing foods to your child’s food repertoire. It takes time, consistency, patience, trust, and so much more.
Keep holiday focus on finding gratitude, spending quality time with family, connecting with community, celebrating with love and joy!
Wishing you and your family a very merry, healthy, happy, and joyous holiday season!
Want more tips? Grab the free guide:
The Dos and Don’ts for Parents of Complex Picky Eaters
GFCF Diets, Picky Eating, Autism, & Other Neurodevelopmental Disorders...What's the Connection? [Blog]
Have you considered starting an elimination diet or some type of special diet for your child and family?
Gluten free. Casein free. Soy free. Paleo. Autoimmune Paleo. Gut and Psychology Syndrome Diet. Specific Carbohydrate Diet. Low Oxalates. Low FODMAPS…
It’s a lot to sort through! That’s why having a trusted resource for nutrition guidance during your child and family’s health and wellness journey can save you time and energy in the long run.
My work with families focuses on guiding parents through special diets and holistic nutrition, while navigating developmental, feeding, and mealtime challenges through the transition.
While I discourage blanket statements or “one-size-fits-all” approaches, most of the children I see benefit immensely from a gluten and casein free diet as a starting point for some extensive time. In fact, some biomedical functional doctors who see children with ASDs or ADHDs will not see the child until they are on a gluten and casein free diet. It’s that foundational for many of these children!
Gluten and casein free diets are not only beneficial to children with autism and neurodevelopmental disorders, but also to many children with severe self-restricted eating habits.
There are many complex picky eaters, with and without neurodevelopmental disorders (NDDs), who have biochemical components involved in their “picky eating” that cause addictive cravings to gluten and casein (and often other foods). While the research is still emerging, my experiences with clients continue to “wow” me with their results and reported improvements! I want to shout this information from the rooftops!
Many of the children I see are sensitive to gluten and casein, sometimes among other chemicals and compounds within foods (amines, glutamates, salicylates, oxalates, etc.), often without their well-intentioned parents being fully aware of foods’ impact. While a variety of food allergy and sensitivity/intolerance testing exists, the best way to determine is often through mindful and guided elimination and reintroductions.
What are gluten and casein?
Gluten is the name of a protein group found in wheat, barely, rye, spelt, and oats that aren’t certified gluten free.
Most people are familiar with gluten and celiac disease, where the individual has an autoimmune disorder response to gluten, and it triggers an antibody response to target person’s small intestinal lining tissue. Notably, children with Down syndrome are predisposed to celiac disease.[1]
There’s also a widespread increase of non-celiac gluten and/or wheat intolerance today.[2] This is where an individual would have a delayed immune system response to gluten protein. It causes an immune system response somewhat similar to an IgE response or a true food allergy, but differing primarily in the severity of the reaction.
A gluten intolerance (and all food intolerances) are not as immediate or life threatening as a true food allergy. Food intolerances and/or food sensitivities, are slower to show and very often overlooked! A “low level” inflammation.
Casein is a family of related proteins found in dairy products.
Casein sensitivity is different than lactose intolerance, although the two can coexist. Molecularly, casein and gluten look similar from our body’s point of view. Both in excessive amounts can cause inflammation, not just for kids on the spectrum but for everyone! [3][4]
Children on the spectrum, as well as other neurodevelopmental disorders, tend to be in a chronic state of low-level inflammation. This is a critical piece of the puzzle to consider, starting with their dietary and lifestyle needs.[5]
A gluten free, casein free diet alone isn’t going to make as big of an impact on health and development as a healthy gluten-free, casein-free, soy-free diet (HGCSF)
Per 2018 study by Dr. James Adams and team, “Comprehensive Nutritional and Dietary Intervention for Autism Spectrum Disorder—A Randomized, Controlled 12-Month Trial”, guidelines for a healthy GCSF diet consist of:
Healthy Gluten-free, Casein-free, Soy-free Diet Guidelines:
Adequate intake of a variety of vegetables (including leafy greens) and fruit (preferably whole fruit). [organic when possible]
Adequate protein quality and intake.
Adequate, but not excessive, caloric intake.
Minimal consumption of “junk” foods and replacement with healthy snacks.
Healthy, gluten-free, casein-free, and soy-free (HGCSF).
Avoidance of artificial flavors, colors, and preservatives.[6]
One of my nutrition teachers, Julie Matthews, was one of the two nutritionists involved in this remarkable study. She has written a comprehensive breakdown of the results, as the study itself is quite lengthy and detailed.
“This study supports what many practitioners and parents have been seeing in practice all along. Finally, we have conclusive evidence that nutritional and dietary intervention is effective at improving non-verbal IQ, autism symptoms, and developmental age in children and adults with ASD!
There were improvements in anxiety, mood, aggression, hyperactivity, focus, and more!
Thus, I’m thrilled to share the results of this 1-year comprehensive study with all of you. The outcomes were life changing for many of the children that participated, and their families and communities, too.”
Read more about it from Julie here [7]
This study is groundbreaking and one of the best out there to show the efficacy and power of nutrition and supplementation on autism. Amazing!
While this study above is specific to autism, it is my professional observations and experiences, these results can be replicated in demographics beyond those with ASDs, to all children with neurodevelopmental disorders and comorbid health conditions.
There are many children who are complex picky eaters that benefit tremendously from a diet of this nature, who do not have a clinical presentation of ASDs or NDDs.
Notice the study above also removes soy from the diet. I also encourage my clients to remove soy as well, if it feels manageable to them. Depending on where they’re starting, if soy is easy to remove initially, then I encourage it.
Soy can be inflammatory for various reasons as well, similar to the gluten and casein proteins. Gluten, casein, and most forms of soy can be over neuroexcitatory for individuals with complex picky eating, autism, and neurodevelopmental disorders.
Considerations before starting the gluten and casein free diet:
While it’s not required, I like to advise my clients to consider biomarker testing before starting the diet.
Once you start the elimination phase of the diet, the tests for celiac disease and food intolerances/sensitivities will likely not be accurate baseline readings (a true look at where you’re starting). If the black and white baseline data matters to you, explore testing options with your child’s team.
Try to get what testing you can through your insurance coverage and your child’s healthcare providers. If possible, an IgE or IgG blood test can be ordered through most pediatricians and family medicine doctors. Note: IgE is really looking for true food allergies, an immediate immune system response, while the IgG (intolerances) is more of a delayed antibody response.
Be sure you’re aligning yourself with doctors and practitioners who will work with you and support your journey. Food sensitivity tests should be seen as a tool, but not the full-picture of what’s happening. Some traditional allopathic medicine doctors are hesitant to order these tests because they can result in false negatives and false positives.
Additionally, keep in mind these Ig biomarkers are only testing the antibodies present in response to the proteins in food. Some children are reacting to more than just the proteins, so those foods wouldn’t necessarily show up on these tests (ex: reacting to salicylates in berries).
We are seeing more and more kids who have food intolerances/sensitivities, and their symptoms of inflammation aren’t being recognized for what they are.
Various behavioral, cognitive, and physical symptoms that are really food intolerances.
The other test you may consider running is a celiac disease test before starting a gluten free diet.
The reason for testing before is because once you start the diet, the test results could result in a false negative (saying gluten is okay/tolerable for your child). I didn’t know this when I personally removed gluten and casein from my diet, and so I like to be sure that people know that information going in!
Most experts in the fields of functional nutrition and medicine in autoimmunity and neurodevelopmental disorders, recommend trialing the gluten and casein free diet at least 6 months, regardless of what the test results indicate.
Often the best way that you can really determine the impacts is through elimination and reintroduction, and work with what you observe with your child. Get really in tune with your child, and prepare yourself to feel like a food detective.
If you’re concerned about nutritional status, consult with a professional who can guide you through it! I’ve seen the diet improve children's health and development in so many ways! Adults too. I often hear that parents and siblings see improvements in their health and wellness while working with families.
5 Connections to Explore When Adopting a Healthy GFCF Diet & How it May Help Improve Your Child’s Picky Eating and Neurodevelopment:
This list is obviously not exhaustive, there are a variety of reasons this diet is beneficial and the starting foundational step for generally many other special diets that someone may eventually progress to.
1. Supporting the repair of the gut lining and blood brain barrier
As I mentioned earlier, there is molecular similarity of the gluten and casein proteins. There is also similarity between the cells of gut lining and the blood brain barrier.[8]
Children with autism, neurodevelopmental disorders, and severely restricted complex picky eating are more likely to have an increased hyper-permeability of the intestinal lining, which places them at risk for weakened blood brain barrier integrity as well.[9]
In infants and very young children, the blood brain barrier is even more vulnerable.
When these barriers are already inflamed or compromised, gluten and casein can be over aggressive, promoting and further exacerbating “leaky gut”/intestinal hyper-permeability.[10]
This hyper-permeability spirals into the creation of more food and environment sensitivities over time, as pathogens and food antigens enter the bloodstream from the digestive tract. The longer it’s left imbalanced and continues to accrue damage, the more symptoms appear and the more difficult it will be to resolve. This is directly triggering the immune system to respond with antibodies against the proteins, gluten and casein.[11]
Healing and sealing the gut by allowing it time to heal without these proteins can be correlated to helping slow down the development of further food intolerances and autoimmune cascades.[12]
2. The quality of our food today...it isn’t “like it used to be”
It’s not as simple as just thinking about this in terms of gluten and casein protein molecules, unfortunately. That’s why I was sure to highlight the 2018 study above [6] and importance of a healthy gluten and casein [and soy] free diet.
We need to also consider the food quality these children are eating. Our wheat today is so very different than the wheat consumed generations ago. For starters, we aren’t soaking or sprouting wheat, rendering it much less digestible to begin with.
I cannot stress enough, the importance of aiming for organic options whenever possible to avoid agricultural residue chemicals, like glyphosate based herbicides and genetically modified (GMO) foods.
While the U.S. isn’t currently producing GMO wheat (to my knowledge/last I knew), essentially all conventionally grown wheat that is harvested in the U.S. is sprayed with glyphosate based herbicides as a drying agent before harvest. It cannot be washed off!
This is another topic to dive into at another time. In the meantime, I highly encourage you to check out the Healing Hope Tribe podcasts with Jessica Eberhart of @Momcologist_On_A_Mission about Glyphosate.
3. An “Opioid Crisis” in our kids?
Could your child be “addicted” to their favorite foods?
Another reason to consider gluten and casein free diets is the Opioid Excess Theory.[14] I find this very fascinating clinically, and I hope to see more and more research emerge on the biochemical mechanisms.
In short summary, when gluten and casein protein molecules are not being properly digested and broken down, they enter the bloodstream and are able to migrate to the brain and central nervous system, inserting into receptors that can cause a myriad of behavioral and/or physical symptoms.
While this research is specific to autism, I think it’s really important to highlight how this theory could be impacting many children, particularly those with complex picky eating (especially those limited to mostly gluten and dairy containing foods) as well as those with neurodevelopmental disorders and special needs.
“The main premise of this theory is that autism is the result of a metabolic disorder. Peptides with opioid activity derived from dietary sources, in particular foods that contain gluten and casein, pass through an abnormally permeable intestinal membrane and enter the central nervous system (CNS) to exert an effect on neurotransmission, as well as producing other physiologically-based symptoms.” [15]
I’ve seen many children, toddlers especially, who have not had a diagnosis or presentation of autism or other NDD, but they had complex restricted picky eating. As demonstrated throughout my work, there are many reasons why a child will exhibit picky eating (sometimes developmentally appropriate picky eating, sometimes not).
The children whose parents come to me and share, “They only eat a few foods...pizza, mac & cheese/noodles, and nuggets” (most commonly), are the children that often respond pretty quickly to nutritional changes!
Not only could their bodies be craving the gluten and dairy because of the opioid excess response, but often these foods in their conventional highly processed forms have artificial food additives and chemicals that could also be causing an addiction like craving.
As their diets are “cleaned up” and the antibodies to gluten and casein leave the body, most children will experience a remarkable expansion in their accepted food repertoire.[16]
4. Consider that your child’s GI issues may not be separate from their behavior, development, and overall well-being.
Improvements in digestion and relief from symptoms of gastrointestinal disorders are also reported benefits of children and individuals on a healthy GFCF diet.[17]
Further thoughts on the opioid excess theory; what digestive symptom is notoriously correlated as a side effect of opioid medications? Constipation!
Many children who are complex picky eaters or who have neurodevelopmental disorders experience a comorbid constipation, diarrhea, and/or alternation between the two.
This can be especially challenging when your child has a hard time with communication. Some children will posture and hang over furniture (or their parents bodies) for pressure on their stomachs, as an adaptive pain relief attempt.
If a child is feeling uncomfortable or they’re in a chronic state of inflammation, it’s very possible that they may experience increased anxiety, sensitivity (environmentally and emotionally), and more. Countless parents have told me that their child’s personalities literally improved. “They are so much more resilient and easy going” or “We were shocked that she just ate what we served!”
Once more, I don’t want to make “blanket statements”. Honestly though, a GFCF diet as a starting point (even if temporary) has time and time again been anecdotally reported to bring a wide variety of improvements to children and families around the world.
A 2009 Parental Survey of over 27,000 parents by the Autism Research Institute found that 69% of parents felt that their children “Got better” on a GFCF diet.[18]
It’s worth considering a healthy GFCF diet as a foundational starting place for families exploring biomedical treatments, including holistic functional nutrition and lifestyle interventions.
5. Reducing gluten and casein can reduce the autoimmune response or potential for developing one, and overall inflammation.[19]
This goes back to the points above related to “heal and seal” the gut lining and blood brain barrier, in order to prevent these proteins from being in the bloodstream (outside the digestive tract) in the first place.
Are you convinced of the incredible potential yet? This is a key reason to consider a healthy, nutrient dense, gluten and casein free diet.
For some children and individuals, not only those on the spectrum, gluten and casein molecules can initiate the body’s immune system to respond against itself. Going after the body’s own proteins!
Symptoms of this autoimmune response on the surface can be seen as behavioral symptoms, especially in young (and pre-verbal) children, if clinicians aren’t certain what signs and biomarkers to explore are a root cause.[20] [21]
For children with autism and neurodevelopmental disorders, the first step is often developmental therapy interventions (speech-language/feeding therapy, occupational therapy, physical therapy, behavioral therapy). These are wonderful services, please don’t get me wrong. Before transitioning into only seeing clients through Speaking of Health & Wellness, I was an Early Intervention Speech-Language Pathologist / Feeding Specialist, and I truly loved serving this age group.
I reached a point in my personal journey where I couldn’t stop thinking, “What if we looked at these conditions differently and as whole body conditions?”
What if the first step was to consider how to bring their central nervous systems into better balance through diet and lifestyle interventions, prior or in tandem to traditional therapies?
Could they be in a better cognitive “space” or disposition to fully receive the benefits of therapies to their maximum potential (vs when they’re clearly dysregulated)?
Absolutely.
Is the GFCF diet “all or nothing”? What happens if they accidentally eat something that isn't GFCF?
I’ll get right to the point; it must be all or nothing at first...for a while!
If you are planning to transition to a GFCF diet, I suggest adopting it gradually for your child. Expect it to take time just to transition fully to having a healthy GFCF diet. This not something that is easily done over night.
When you finally reach the stage of your child eating a completely GFCF diet, mark your calendar or make a note. From there, it’s widely suggested it can take at least 6 months minimum to judge it’s effectiveness.
I believe it’s worth full commitment for a year and then reassess. Note once again, that one of the best studies out there on this topic is the 2018 study showing great health and developmental improvements after a full year of dietary intervention and supplementation![6]
Generally speaking, it’s estimated that it takes:
~3 weeks of complete elimination for casein antibodies to leave the system
~4-6 months of complete elimination for gluten antibodies to leave the system
So really, you can’t judge the true effectiveness of the diet until 6 months, no “oops moments”. I will never forget watching an online interview during my own health journey, where autoimmunity expert, Dr. Amy Meyers, said that even just one bite of gluten can send your immune system into trigger for 4-6 months, even when you’ve been gluten free. Yikes!
A decent portion of the previously conducted literature on the GFCF diet, especially those studying the diet's impact on autism, were not trialed long enough.
A few days or weeks to evaluate the true capacity of a healthy GFCF diet on your child’s health and development is simply not long enough. Further, many of these studies also are not using healthy GFCF diets. Sometimes they’re even using gluten free or casein free exclusively, not mutually.
When journalists or the mainstream media are discrediting the impacts of GFCF diets (on autism typically), look closer at the studies being cited. Are they studies with short trial periods? Are they really following a healthy gluten and casein free diet? More often than not, it’s not the full picture.
Thankfully, through parents telling their family’s stories and collaborating with functional practitioners and providers around the globe, the paradigm is shifting.
The 2018 study by Dr. James Adams and team cannot be over-celebrated! It’s truly groundbreaking and well-worth the print and read. It would also be advantageous to look deeper into the exceptional work of the involved contributors.
Mistakes are bound to happen…
Here’s what to do when there’s an “oops moment” with the diet:
- First, take a deep breath in…and out…
Now, mindfully observe what happens.
What behavioral and/or physical symptoms appear related in the days following?
Watch for a full week. Are they more irritable? Whiney? Clingy? Craving / asking for their offending foods? More spacey? Less engaged? Constipated? Diarrhea? Any skin rashes or bumps?
Write it all down. This will help you and your child’s team identify offending food “triggers” and patterns over time.
Look into these supports to have on hand when there has been a diet infraction:
Speak with your child’s providers to see what follow up they’d specifically recommend as well.
Activated charcoal
DPP-IV Enzymes (Klaire Labs Chewables, Ezymedica, Houston Enzymes are generally my go-to recommendations for clients)
Magnesium or Epsom Salt Baths
Increased hydration
Lemon water
- Start again.
Don’t let the mistake get you down. Mistakes will happen!
Accept that right now and learn to look for the lessons. Use it to your advantage to observe and fuel your why, why you’re implementing the diet in the first place.
Many parents have shared with me that this is when they get the real “buy in from the non-believers” around them, when there’s an oops moment at a birthday party or with grandma or other. Those who are there to witness the child before and after exposure, generally realize quickly, “Wow yeah, I guess [food] really does impact them”.
Not everyone is going to understand or agree with your approach to try diet changes, especially not at first. The more people who are potentially feeding your child, the more grace, patience, and consistency you have to have, expecting that there will be errors. Keep coming back to start, again and again!
- Aim for least restriction with high nutrient density.
We have to remember that just because a food or meal is GFCF, it doesn’t mean that we’re eating “healthy”. Our focus should be shifting to maximize nutrient density and decreasing artificial food additives and agricultural chemical residues.
Just like gluten and casein, these food chemicals like artificial colors, flavors, and preservatives can wreak havoc at the cellular levels, especially in the gut and brain!
And really, that’s one of the biggest points of the diet, is to help heal and seal the barriers of the gut and the brain from our these “invaders” in our bloodstreams. If we’re only removing gluten and casein but not continuing to improve overall quality of their diet, then families will be missing opportunities for further or faster healing of the gut.
It’s a slow and steady process. It’s not done overnight, especially if your child is starting with only consuming highly processed, primarily gluten and dairy containing foods. I encourage parents to try a food-first focussed approach for nutrients whenever possible, but the truth is many of these children are deficient in certain nutrients already, so some guided supplementation can be really helpful.
I always tell my clients:
We are working towards the most nutrient dense and least restrictive diet that we can get your child to willingly accept.
How do you know if they aren’t getting all the nutrients they need?
You can hypothesize through symptom observation but the best way to know if they aren’t getting all their nutrients is through assessment. There are various assessments, some more formal than others (food journals vs. labs, etc.). Some more credible than others.
Some basic labs for biomarkers may be available for coverage through insurance with their pediatrician (IgG and IgE, for example). Other labs may have to be ordered through a functional medicine doctor or nutritionist. Direct to consumer labs exist for access as well.
Some nutrients can be informally measured at home, like zinc.
The zinc assay taste test is a popular at home test I often suggest to parents try.[22] Zinc deficiency alters the sensory perception and experience of taste and smell, which can create food aversions.[23]
I find this to be a very common deficiency in the population of children I’m serving with complex picky eating, with and without neurodevelopmental disorders.
Interestingly, zinc deficiency has been observed in patients treated with opioid medications, and it’s supplementation has been used for opioid addictions.[24]
I find this really fascinating given what we know about gluten and casein proteins creating opioid responses and addictive cravings, often in the presence of children with simultaneous zinc deficiency!
What about calcium?
Calcium...everyone’s big question when you remove casein / dairy from the diet.
Calcium is a very important macromineral, but it’s important to note that you don’t want to go mega dosing on calcium in isolation because your child is dairy free.
Honestly, we aren’t really getting that much absorbable calcium from cow's milk and there are many non-dairy foods that contain calcium sources (sardines, broccoli, bok choy, pumpkin seeds, etc.).
Calcium is a “game of co-factors” as you’ll hear fellow Nutritional Therapy Practitioners say. Calcium absorption, assimilation, and utilization in the body depends on and requires 7 co-factors for proper absorption, as outlined by The Nutritional Therapy Association below.
I think it’s critically important and worth noting, as this is one of the most common questions related to use of GFCF diets.
Calcium requires 7 co-factors for proper absorption (notes from Nutritional Therapy Association):
Systemic pH
Hormonal functioning
Hydration (water & electrolytes)
Balance with Other Minerals
Vitamin D
Fatty Acids
Needed to transport of calcium into the cell
Digestion
Calcium is only absorbed in an optimally acidic environment and requires HCl (stomach acid) for uptake
To keep it simple, most individuals are taking in enough calcium but the question is: Are they properly absorbing it and if not, why? If they aren’t, do they have the required co-factors to properly assimilate calcium? Because that needs to be explored in addition to adding in supplementation as appropriate.
I sometimes suggest a high quality, food based, mutli-vitamin for a few months to give a general overall boost through initial diet transition, then re-test and see. We always want to be sure there aren’t synthetic or unnecessary fillers, artificial colors or flavors, for these very sensitive children.
Autism Nutrition Research Center Essentials Plus Powder is a great option that we know is research based. After the 2018 study I previously mentioned on the impacts of a healthy, gluten, casein, and soy free diet was completed, the supplement used in the study was re-formulated and improved based on their findings.[6] (Dr. James Adams does not receive monetary reimbursement from the sales of this supplement, nor do I).
Garden of Life MyKind Gummies are a reasonable option too, as a starting point. These are conveniently found at most Whole Foods stores. Klaire Labs Vita Spectrum is another quality multivitamin that some of my clients have used and liked.
If you’re needing more guidance and reassurance on calcium, ask your provider about lab testing, and if supplementing with calcium in isolation is necessary (and which forms they recommend). If isolated calcium supplementation is needed, citrate or malate calcium forms seem to be the most widely tolerated and recommended among this population of children from what I’ve gathered.
Be aware, some calcium citrate supplements are GMO corn derived.
Is this diet change temporary or a life long commitment?
It’s hard to really say for sure.
It depends on your child, the individual.
We are really just starting to see the first major wave of adults with autism come through today. Many of them aren’t currently on and/or were not on specialized diets growing up and because of funding allocations for research, we don’t have a lot of actual data to answer this specifically regarding children on the spectrum and/or who have other neurodevelopmental disorders.
My guess though is that for some it may be temporary, but for most, it’s likely going to be something they follow for years, possibly lifelong. Especially in regards to gluten elimination. It’s very child dependent based on where they’re starting, what they’ve been eating, and what they eat while on the GFCF diet. How much “gut healing” has taken place? Has their immune system and nervous system settled and regulated? There are a lot of variables to consider for each bioindividual child.
Here’s the thing, GFCF is really just the tip of the iceberg. Many of these children need a bio-individualized diet tailored to them far beyond GFCF. If a remarkable amount of biochemical healing and improvement occurs, especially in the gut, then perhaps these children could grow into teens or adults who could occasionally tolerate gluten and/or casein containing foods in moderation.
Everyone is different and we’re still learning so much about the intricate impacts of diet, nutrition, and supplementation as a scientific and medical community.
Oftentimes, once gluten and casein are removed then you can really see the other foods that were triggering them as well. For example, red apples or tomatoes may not have been an obvious issue before, but after being GFCF for some time you may start to think they’ve developed new sensitivities. It may not necessarily be that the sensitivities are new, it may be that they were hidden. Masked food sensitivity symptoms beneath the gluten and casein reactions.
From what I have gathered, it seems some children are able to tolerate casein occasionally (in certain forms) after working on their gut healing and food intolerances for an extended period of time. Ex: Goat’s milk and camel’s milk are easier to digest than cow's milk, and raw cow’s milk is more digestible than pasteurized cow’s milk.
It will depend on their individual reasons why gluten and casein molecules caused challenges for them initially, and how this was followed up.
I would be interested to see more long term testimonials and higher level research on GFCF diets. From the research I’ve personally read and the work I’ve done with clients, I would advise families to expect that gluten likely needs to remain out of the diet for a long time.
Going back to those inevitable “oops moments” of diet infractions, parents are able to see how these foods are causing them to react (or no longer react). Sometimes it’s very obvious they aren’t able to tolerate it still, and the diet is worth continuing. Sometimes the child, if they’re old enough and able to understand, is also able to connect the food intolerance/sensitivity symptoms.
I don’t want to be too “all or nothing” though. Diet is always very bioindividual, I just don’t want to give a false hope either that after a year or two your child will be able to eat gluten and casein without an issue... Unfortunately that hasn’t been the experience I’ve seen, but I would confidently say all of my clients would tell you that it’s worth it!
How long should it take to see results?
Generally speaking, most of my clients see beginning results within the first 2-3 weeks.
Some parents may see some progress at about a week or so, but it depends if you’re starting with gluten, or with casein, or with both at the same time, and how exactly you make the transition.
Keeping in mind that, “Sometimes things get worse before they get better”. If a child has strong addictive like cravings to gluten and casein, you may see very strong willed behaviors from your child as they initially adjust.
Parents have reported statements along the lines of, “After [that initial adjustment stage], it’s like a light turned on / a fog cleared up / a veil was lifted.” It’s impeccably rewarding to be a part of helping parents attain such progress, and create these changes for their child’s health and development.
Give the complete healthy gluten and casein free diet (and soy free if possible), at least 6 months with zero “oops moments”.
If there is an “oops moment”, make a note and do a mental reset of the diet. Or maybe not a full reset, depending how long your child has been on it and how much gluten or casein they ate, and what their reactions were. At the very least make note of it. And then start again.
Gluten and dairy free diets are foundational to most special diets focused on improving the integrity of the gut lining and minimizing food reactions.
Is it a fix all or magic cure? No! Absolutely not, but it’s always worth exploring for complex picky eating, autism, and neurodevelopmental disorders. These children have quite a bit in common from a biochemical bio individual perspective.
General Habits and Guidelines for Families to Embrace During the GFCF Diet Transition:
- It’s critical that everyone in the family (and who feeds the child) is on the same page, and supportive at the very least.
Best results come from families who are implementing the diet together, eating the same family meals.
- During the initial transition, consider improving the quality of the family’s favorite foods first.
Adding before removing. This way you’re focused on adding and what they can have, before removals! Cookies to organic cookies. Mac and cheese to organic Mac and Cheese. Chips to organic chips.
Choosing the healthier version that's organic when possible, always free of GMOs, agricultural toxicant chemicals, factory farmed animals or their by-products.
One swap at a time, focused on improving quality. If it’s gluten and dairy free, that’s even better!
- Slowly but surely, while you’re swapping the swaps for cleaner versions of your family’s favorites, start removing gluten and dairy.
Overtime, become more mindful of lowering refined sugars. This will happen somewhat naturally, secondary to the steps mentioned above. Then eventually, consider removing all refined sugars, even organic.
- When this feels sustainable, start expanding to minimal ingredients and more whole food focused recipes to increase nutrient density.
Ex: Maybe the Organic GFCF Mac and Cheese is replaced with one ingredient organic rice flour noodles and the "cheese" is made homemade from butternut squash, or cashews, or coconut yogurt and nutritional yeast (non-fortified only: Sari Foods is my go-to due to MTHFR genetic mutations, and note that some children with yeast don’t tolerate this well).
- Ask for support when and where you need it
If you need support with your child’s complex picky eating, autism symptoms, or neurodevelopmental needs, and are considering a healthy gluten and casein free diet, don’t hesitate to reach out! I would be honored to support you through the transition.
If you’re not reaching out to me, reach out to someone else you trust for support.
- Lastly, have grace, patience, and consistency with the process and everyone involved. Including you!
Change does not happen over night. Don’t give up! For most families it really, truly, is worth it.
GRAB YOUR FREE GUIDE:
The Dos and Don’ts for Parents of Complex Picky Eaters
Celiac Disease Foundation Website https://celiac.org/about-celiac-disease/what-is-celiac-disease
Barbaro, M.R., Cremon, C., Stanghellini, V. and Barbara, G. (2018). Recent advances in understanding non-celiac gluten sensitivity [version 1; peer review: 2 approved]. F1000Research, 7(F1000 Faculty Rev):1631 (https://doi.org/10.12688/f1000research.15849.1)
Vojdani, A. (2015). Molecular mimicry as a mechanism for food immune reactivities and autoimmunity. Alternative therapies in health and medicine, 21 Suppl 1, 34–45.
Hollon, J., Puppa, E. L., Greenwald, B., Goldberg, E., Guerrerio, A., & Fasano, A. (2015). Effect of gliadin on permeability of intestinal biopsy explants from celiac disease patients and patients with non-celiac gluten sensitivity. Nutrients, 7(3), 1565–1576. https://doi.org/10.3390/nu7031565
Luna, R. A., Oezguen, N., Balderas, M., Venkatachalam, A., Runge, J. K., Versalovic, J., Veenstra-VanderWeele, J., Anderson, G. M., Savidge, T., & Williams, K. C. (2016). Distinct Microbiome-Neuroimmune Signatures Correlate With Functional Abdominal Pain in Children With Autism Spectrum Disorder. Cellular and molecular gastroenterology and hepatology, 3(2), 218–230. https://doi.org/10.1016/j.jcmgh.2016.11.008
Adams, J.B.; Audhya, T.; Geis, E.; Gehn, E.; Fimbres, V.; Pollard, E.L.; Mitchell, J.; Ingram, J.; Hellmers, R.; Laake, D.; Matthews, J.S.; Li, K.; Naviaux, J.C.; Naviaux, R.K.; Adams, R.L.; Coleman, D.M.; Quig, D.W. Comprehensive Nutritional and Dietary Intervention for Autism Spectrum Disorder—A Randomized, Controlled 12-Month Trial. Nutrients 2018, 10, 369.
Matthews, J. (2020). Autism symptoms improve with better diet and nutrition, 1-year study concludes. Retrieved from https://nourishinghope.com/autism-symptoms-improve-with-better-diet-and-nutrition-1-year-study-concludes/
Daneman, R., & Rescigno, M. (2009). The gut immune barrier and the blood-brain barrier: are they so different?. Immunity, 31(5), 722–735. https://doi.org/10.1016/j.immuni.2009.09.012
D'Eufemia, P., Celli, M., Finocchiaro, R., Pacifico, L., Viozzi, L., Zaccagnini, M., Cardi, E., & Giardini, O. (1996). Abnormal intestinal permeability in children with autism. Acta paediatrica (Oslo, Norway : 1992), 85(9), 1076–1079. https://doi.org/10.1111/j.1651-2227.1996.tb14220.x
Hollon, J., Puppa, E. L., Greenwald, B., Goldberg, E., Guerrerio, A., & Fasano, A. (2015). Effect of gliadin on permeability of intestinal biopsy explants from celiac disease patients and patients with non-celiac gluten sensitivity. Nutrients, 7(3), 1565–1576. https://doi.org/10.3390/nu7031565
de Magistris, L., Picardi, A., Siniscalco, D., Riccio, M. P., Sapone, A., Cariello, R., Abbadessa, S., Medici, N., Lammers, K. M., Schiraldi, C., Iardino, P., Marotta, R., Tolone, C., Fasano, A., Pascotto, A., & Bravaccio, C. (2013). Antibodies against food antigens in patients with autistic spectrum disorders. BioMed research international, 2013, 729349. https://doi.org/10.1155/2013/729349
Rudzki, L., & Szulc, A. (2018). "Immune Gate" of Psychopathology-The Role of Gut Derived Immune Activation in Major Psychiatric Disorders. Frontiers in psychiatry, 9, 205. https://doi.org/10.3389/fpsyt.2018.00205
Hande Cekici & Nevin Sanlier (2019) Current nutritional approaches in managing autism spectrum disorder: A review, Nutritional Neuroscience, 22:3, 145-155, DOI: 10.1080/1028415X.2017.1358481
Reichelt, K. L., Tveiten, D., Knivsberg, A. M., & Brønstad, G. (2012). Peptides' role in autism with emphasis on exorphins. Microbial ecology in health and disease, 23, 10.3402/mehd.v23i0.18958. https://doi.org/10.3402/mehd.v23i0.18958
Whiteley, P., & Shattock, P. (2002). Biochemical aspects in autism spectrum disorders: updating the opioid-excess theory and presenting new opportunities for biomedical intervention, Expert Opinion on Therapeutic Targets, 6:2,175-183, DOI: 10.1517/14728222.6.2.175
Cornish E. (2002). Gluten and casein free diets in autism: a study of the effects on food choice and nutrition. Journal of human nutrition and dietetics : the official journal of the British Dietetic Association, 15(4), 261–269. https://doi.org/10.1046/j.1365-277x.2002.00372.x
Jyonouchi, H., Geng, L., Ruby, A., Reddy, C., & Zimmerman-Bier, B. (2005). Evaluation of an association between gastrointestinal symptoms and cytokine production against common dietary proteins in children with autism spectrum disorders. The Journal of pediatrics, 146(5), 605–610. https://doi.org/10.1016/j.jpeds.2005.01.027
Autism Research Institute (2009) Publ. 34/March 2009. Parent Ratings of Behavioral Effects of Biomedical Interventions. Form 34QR March 2009 - all.pub
Vojdani, A. (2015). Molecular mimicry as a mechanism for food immune reactivities and autoimmunity. Alternative therapies in health and medicine, 21 Suppl 1, 34–45. https://pubmed.ncbi.nlm.nih.gov/25599184
Casella, G., Pozzi, R., Cigognetti, M., Bachetti, F., Torti, G., Cadei, M., Villanacci, V., Baldini, V., & Bassotti, G. (2017). Mood disorders and non-celiac gluten sensitivity. Minerva gastroenterologica e dietologica, 63(1), 32–37. https://doi.org/10.23736/S1121-421X.16.02325-4
Lionetti, E., Leonardi, S., Franzonello, C., Mancardi, M., Ruggieri, M., & Catassi, C. (2015). Gluten Psychosis: Confirmation of a New Clinical Entity. Nutrients, 7(7), 5532–5539. https://doi.org/10.3390/nu7075235
Zdilla, M. J., Starkey, L. D., & Saling, J. R. (2015). A Taste-intensity Visual Analog Scale: An Improved Zinc Taste-test Protocol. Integrative medicine (Encinitas, Calif.), 14(2), 34–38. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4566477/
Takakazu Yagi, Akihiro Asakawa, Hirotaka Ueda, Satoshi Ikeda, Shouichi Miyawaki and Akio Inui, “The Role of Zinc in the Treatment of Taste Disorders”, Recent Patents on Food, Nutrition & Agriculture (2013) 5: 44. https://doi.org/10.2174/2212798411305010007
Ciubotariu, D., Ghiciuc, C.M. & Lupușoru, C.E. Zinc involvement in opioid addiction and analgesia – should zinc supplementation be recommended for opioid-treated persons?.Subst Abuse Treat Prev Policy 10, 29 (2015). https://doi.org/10.1186/s13011-015-0025-2
Advice to Parents of Children with Dyslexia, From Adults Who Have Dyslexia.
The two women I love most in this world, my mother and younger (only) sister, both have dyslexia.
With their permission and October being Dyslexia Awareness Month, as we wrap up the month I want to bring awareness to dyslexia by sharing a bit of their experiences and advice.
I polled my instagram audience on what questions they’d want to ask an adult with dyslexia and a mother of a child with dyslexia. The questions were all so good! I narrowed it down to the few that were the most recurring in nature.
My hope is that this reaches a parent of a child who has dyslexia and gives you a variety of perspectives and tips to consider.
A perspective that can only come from the adults living with the same condition. As well as a perspective that only a daughter and sister of someone living with dyslexia can offer. Similarly, keep in my that I'm a speech-language pathologist which also offers another unique angle to my own perspective.
“Dyslexia” falls under the umbrella diagnostic term of Specific Learning Disorder (SLD) which is a classification of a Neurodevelopmental Disorder (NDD). It’s important to note that both learning disorders and cognitive disorders fall under the umbrella of NDDs, but these are different conditions. A child with an SLD will not necessarily have dyslexia, but dyslexia falls within SLD category.
For their privacy, I will refer to them as “My Mom” and “My sister” throughout this blog.
When I pitched the idea of interviewing them both, my Mom was super open to it as I expected. I wasn’t sure how my sister would feel about it. I am grateful for each of their vulnerability and willingness to be open and reflective with me for this collaboration! Additionally, I am grateful that you have taken the time to read more about dyslexia and the two women I love most.
My Mom and sister are both brilliantly bright and passionate women.
As you might expect, the topics and areas they are passionate about are where they excel. They can both rattle off facts on facts for days about what they love and what genuinely lights them up!
For both of them, especially my sister, it’s horses. Horses have been their bond over the years and they both have this indescribable fearless grace, a “horse sense” that blows my mind.
My Mom can identify all sorts of trees, plants, dogs, horses, and wild animals. She can shout out the year of old car models when she sees them. Both of their intelligences are “normal” but their reading and writing are challenging. For example: I will be calling her to read this blog post to her once published and she’ll read along (or not) while I read it outloud.
My Mom doesn't like to read or write in long lengths because it’s a struggle for her, but she’s learned how to compensate for the areas she needs help with in her life. Shout out to my Dad for being the prominent person to help when and where she needs support. (He deserves recognition here too for his support of course!) My Mom’s dyslexia is more severe than my sister’s.
My sister is a poetic and gifted writer, a talented artist, guitar player, and all around made of pure magic. Every year I watch her step more into herself and grow into a young woman is a privilege. I have tears in my eyes writing it. She’s still learning her full greatness each day but my parents and I have always felt it.
I think you get the point here - I want you to know that dyslexia is just one piece of who they are. It is not who they are. I am intentionally using “first person language” (ex: “person with dyslexia” vs. “dyslexic person”) for those very reasons.
They happen to have dyslexia but they are not their diagnoses.
Please remember this when thinking of your children (and how you and others speak about them in front of them).
It is my honor to share their experiences to shed light on living with dyslexia.
Without further ado, let’s dive into my brief interview with each of them…
I texted my Mom a few questions to think about and told her she could text me back or we could talk about it. The process of typing her replies is too tedious and cumbersome, so she preferred to have me call her.
We spoke for about an hour and she told me stories that I hadn’t heard before. Including one where she was bullied and humiliated as an adult (like middle school style bullying) at a job for her spelling errors in front of the team. I was furious and hurt for her. I can’t imagine the audacity of these other adults...or how that must have made my Mom feel as a grown woman who thought she was done being bullied for learning differently.
She also enlightened me on some of her self talk and affirmations that she’s had on mental repeat and grown into over time. Below are her answers and takeaway messages paraphrased from our conversation.
What are the top tips you would tell a parent of a child who has dyslexia?
“Be patient and understand that your child learns differently”
“Find their strengths and maximize what they love when they’re struggling to learn”
“Recognize when they need breaks and what resets them”
“Be their voice and watch closely for overwhelm in the school system”
We talked about how children’s work loads in schools are already so overloaded. School looks very different than when we were children. When you add a learning disorder on top of that, it can turn overwhelming fast. Especially the transition from elementary to middle school, when academic demands increase.
My Mom emphasized being aware of the various ways that you can advocate for your child within the school even though you’re not there, including by putting IEP accommodations and supports in place. An “IEP” is an Individualized Education Plan that is a legally binding document that a child qualifies for through a Special Education evaluation. Goals and accommodations are discussed based on the child’s needs and grade requirements. This plan is meant to serve as the roadmap to helping the child receive access to fair and appropriate public education, their right by federal law (if qualified).
As a clinician, I always want to empower parents to know and understand that they are just as important of a role as each of the professionals around the table of the IEP meetings. If your child has difficulty with phonology, reading, spelling, writing, etc., that’s all impacting their access to academics! You are able to add in your own ideas and thoughts into the language of the IEP. In fact, you should! They are the experts in their fields but YOU are the expert on your child! It’s up to you to advocate for them and teach them how to be the best advocate for themselves.
You are not required to sign an IEP until you agree with the document. If needed, find an advocate to support you with the school system. Thankfully in my sister’s case, this was never required and the school was always pretty supportive (although, didn’t always fully have the resources which is unfortunately common).
If you could describe your experience while reading and learning, how would you best describe it?
When I asked her this, my Mom sighed a big breath and said,
“Reading...I don’t like to do because I struggle. For me to grasp it, I have to read it over and over and over and over again. People take reading for granted”.
When she said that it hit me deeply. I realized in that moment that I, as her daughter, do in fact take reading for granted too often.
She shared how even jobs that many would consider “simple” would be very difficult for her. Being a waitress, bank teller, cashier, gas station attendant, etc. Anything with reading letters and numbers is challenging, especially in a situation where there would be a time pressure.
My Mom is a trained and experienced dog groomer. We live in a rural area where these jobs aren’t plentiful. When I was growing up, my Mom stayed home and cared for us when we were very young, which I am so thankful for! When my younger sister entered school, my Mom worked as a dog groomer and held other various jobs throughout the years. My Mom learned to maximize her strengths throughout her life for the jobs she’s held. She’s very in tune with animals and is an incredibly patient woman, and a selfless caregiver. She has held roles caring for animals and people in varying capacities.
We discussed the idea of dyslexia being popularly simplified as “reading backwards”. Like my sister has also described to me: It’s not that they’re reading backwards, it’s that the letters and numbers “jump and scramble”. For example, my Mom almost always writes “talk” as “tlak”.
As a speech-language pathologist, I can’t help but be able to reflect on the language and phonological components of how she is receiving and expressing written language. I can only have sincere empathy for her experience, as I imagine it would be frustrating to experience throughout your life. I know it has been for her and I’m inspired by the way she doesn’t allow it to limit her in any way.
She took me to the library a lot as a child. During our call, she told me she always felt I was “in tune” with her. As I became a better reader than her growing up, she realized I was in tune with where/when she needed help with various tasks requiring reading and writing.
What strategies and strengths do you use in your daily life for your success? (Direct Quotes)
“I’ve learned not to be afraid to ask for help when I need it. I try not to make excuses for myself and recognize when I am.”
“I’ve realized I need to slow myself down and remove myself from situations when possible then re-entering before reacting. Sometimes I need to shut my brain off for a second and let it catch up with itself”
“I make lists and write things down a lot.”
My Mom leaves herself notes to remind her to do things and help her remember what order to execute tasks. I do this as well, personally.
She described herself as a very hands-on learner and noted preferring being read to vs. reading herself when learning and testing.
Words of wisdom to others who have dyslexia and/or other learning disorders:
“Don’t beat yourself up and don’t let society tell you that you can’t learn”
“Don’t ever be ashamed of who you are”
“Know you’re different but that’s what makes you you” (the collection of everything about you - not just your learning difference).
“The biggest thing is accepting that you have limitations. I continue to work on this through out my life. Some days it frustrates me so bad. I don’t know if it’s the ADHD or the dyslexia, but sometimes my brain feels like it’s going faster than the body can handle.”
Without going into detail, I also want to note from an epigenetic perspective that my Mom’s childhood was not “all sunshine and roses”. She grew up in a home with limited resources and not the best nutrition for the beginning of her life. Additionally, she experienced events that would make anyone “grow up” faster than a kid is supposed to.
Knowing what I know professionally, while also being her daughter and knowing all she’s been through, I can’t even begin to articulate how infinitely proud and inspired I am to be her daughter. She’s faced hurdles every day that we can’t really grasp because we don’t live with dyslexia.
Can you imagine triple or quadruple checking everything that you read and wrote?Can you imagine always being self conscious and unable to trust yourself that you’ve read it and/or written it correctly?
My Mom is my best friend and my absolute idol. We have always been incredibly close. I’m blessed to say my family unit as a whole is very strong! We’re all very close despite living in separate parts of the country. My Mom has been a phenomenal guide and role model for my younger sister, who also has dyslexia.
During the call with my Mom she said, “I’m so glad your sister doesn’t have it as severe as I do”. There are so many variables to the spectrum of neurodevelopmental disorders and in this case, consider a spectrum of dyslexia. Imagine the ways my Mom must’ve supported her from a place of true understanding because she knew what it was like first hand.
I have this image of my little sister doing her homework at the kitchen table, slamming her pencil down as she bounced up in her chair with a frustration sound…
If I could time travel back, I would hug her and whisper, “Don’t worry - Everything will be okay. Guess what - you’re going to grow up and work with horses like you’ll always dream of, live somewhere warm all year round, and you’ll be the most amazing woman!”
I received my sister’s responses by text and she has given me permission to share her text unedited verbatim. Please keep in mind: She didn’t know that I was going to share in this way, so she may have further edited if she knew that.
We both thought it was appropriate to share her unedited, uncorrected, and natural response in honor of this being a Dyslexia Awareness post.
What are the top tips you would tell a parent of a child who has dyslexia?
“I’d tell the parents that patients is important, they can’t always trust to sound out a word or follow that math equation correctly because eyes lie to them so often.
Also being involved with your child’s school work at home, but also at school.
Sometimes kids don’t know how to be their own advocate and need that extra help. It’s important that the teacher work on different strategies in the classroom because your child may find it hard to follow.”
If you could describe your experience while reading and learning, how would you best describe it?
“The easiest way to describe my reading and learning experience is that I personally do much better with things hands on.
It’s hard to remember orders In which steps to follow.
When I was younger it was complicated and hard to trust anything I put down on paper. In fear that no other person could read and comprehend my work.”
Words of wisdom to others who have dyslexia and/or other learning disorders:
“Over the years I struggled with reading, learning a second language and math. It wasn’t until I got older and learned my own disability and how it worked for me.. to be able to cope with the every day struggle.
You’ve got to stop disliking yourself for being the way it is. Once I excepted that I was dyslexic, i was easier on myself.. though the biggest thing I can’t stress enough is patience.. with your children ^^ and with yourself.
Hope this makes sense and that it is useful. Let me know if you have questions.. Love you Shandy”
When I read her replies it was a couple hours after having the phone conversation with my Mom. There is so much overlap between what my Mom said and her responses. Especially the emphasis of holding patience for yourself and your child, and accepting it vs. making it something negative about yourself.
My eyes welled with tears as I read her answers and thought about how proud and fulfilled our incredible Mother should be for raising such a resilient and radiant soul! My parents and I are so intensely proud of my sister.
My Mom, who happens to have dyslexia, has been happily married to her high school sweetheart and love of her life for over 30 years. They’ve raised two successful children and are doing great!
My sister, who happens to have dyslexia, has a job she loves working with horses and is thriving in the young prime of her beautiful life!
If your child happens to have dyslexia as well (or other learning disorder), I know that you’ve gained inspiration in some way from this blog post.
On the next tough day your little one has, I hope that you will remember this blog post about two women I love most in this world - my mother and younger sister, who happen to have dyslexia.
A gentle reminder from my family to yours:
Be patient with your child and with yourself.
(Couldn’t have said it better Mom and sister! xo)
To my Mom and sister - Thank you for letting me share our interviews and your words here on my site for others to learn. Thank you both for walking this life as your authentic selves and inspiring me to do the same. I’m honored to learn from and share your experience. I’m blessed and grateful for you both! (and Dad! And “the critters!”)
Want to keep learning with me?
Listen in to the podcast:
Exploring Autism & Other Neurodevelopmental Disorders as Whole Body Conditions [Blog]
[Click here to listen to my accompanying podcast, “Exploring Autism & Other Neurodevelopmental Disorders as Whole Body Conditions”]
I will continue to build on this topic but for now (before I get too ahead of myself), let’s get into some foundational information about autism spectrum disorders & other neurodevelopmental disorders as whole body conditions.
I hope that this blog will be a good starting point to help evolve your perception of autism spectrum disorders (ASDs) and neurodevelopmental disorders (NDDs) in general.
ASDs are referred to as “spectrum” disorders to reflect the vast varieties of skills and symptoms of each individual, while also sharing similarities. Most autism researchers agree that we are beginning to be able to recognize different subtype groups of individuals on the spectrum, based on causes, treatments, and related commonalities.
There’s a quote in the world of autism, “If you’ve met one person with autism, you’ve met one person with autism” by Dr. Stephen Shore. Meaning, don’t think that you know what “autism looks like” because you’ve met one or a few children or individuals on the spectrum. I have personally worked with children on the spectrum for a decade and fully agree with this quote in a number of ways.
Since you’re here, you probably already know the common symptoms and signs of ASDs but just in case you don’t, let’s review them briefly.
According to the DSM-5 [1], the diagnostic criteria for ASDs are based upon symptoms/traits that include:
“Persistent deficits in social communication and social interaction across multiple contexts”
“Restricted, repetitive patterns of behavior, interests, or activities.”
“Symptoms cause clinically significant impairment in social, occupational, or other important areas of current functioning.”
For perspective, in the 70s / early 80s, it was said to be at 1 in 10,000 children. According to CDC data, autism spectrum disorders now impact 1 in 36 children [2]...or 1 in 59 [3] depending on which CDC data you chose... That’s a separate blog for a later time.
The point is that we’re at epidemic rates. Rates that are unsustainable for families, our nation, and the world if we are to truly help support these children/individuals and their families obtain the resources and supports they need access to!
Some argue that the rise in diagnosis can be attributed to better diagnosis, earlier diagnosis, and changes in diagnostic criteria. I find this implication oversimplified and relatively dismissive. As a pediatric SLP, I’ll be the first to admit I have witnessed some over diagnosis but the reality is that a change in or increased identification of ASDs cannot account for even half of the increased rates we’ve seen over time. Not only across our country but also around the world.
Per Hertz-Picciotto in a 2009 study published in Epidemiology, earlier diagnosis and changes in diagnostic criteria only accounted for ~1/3 of the increase in total rates of ASD [4].
When I am faced with the “it’s better diagnosis” response, I like to bring the conversation to the bigger picture. The rates of chronic illness in children and adults have increased significantly in the last 2-3 decades. Over half, (~54%) of both children [5] and millenials [6] have a diagnosed chronic health condition. With this information we can reflectively say that society at large is experiencing a health crisis.
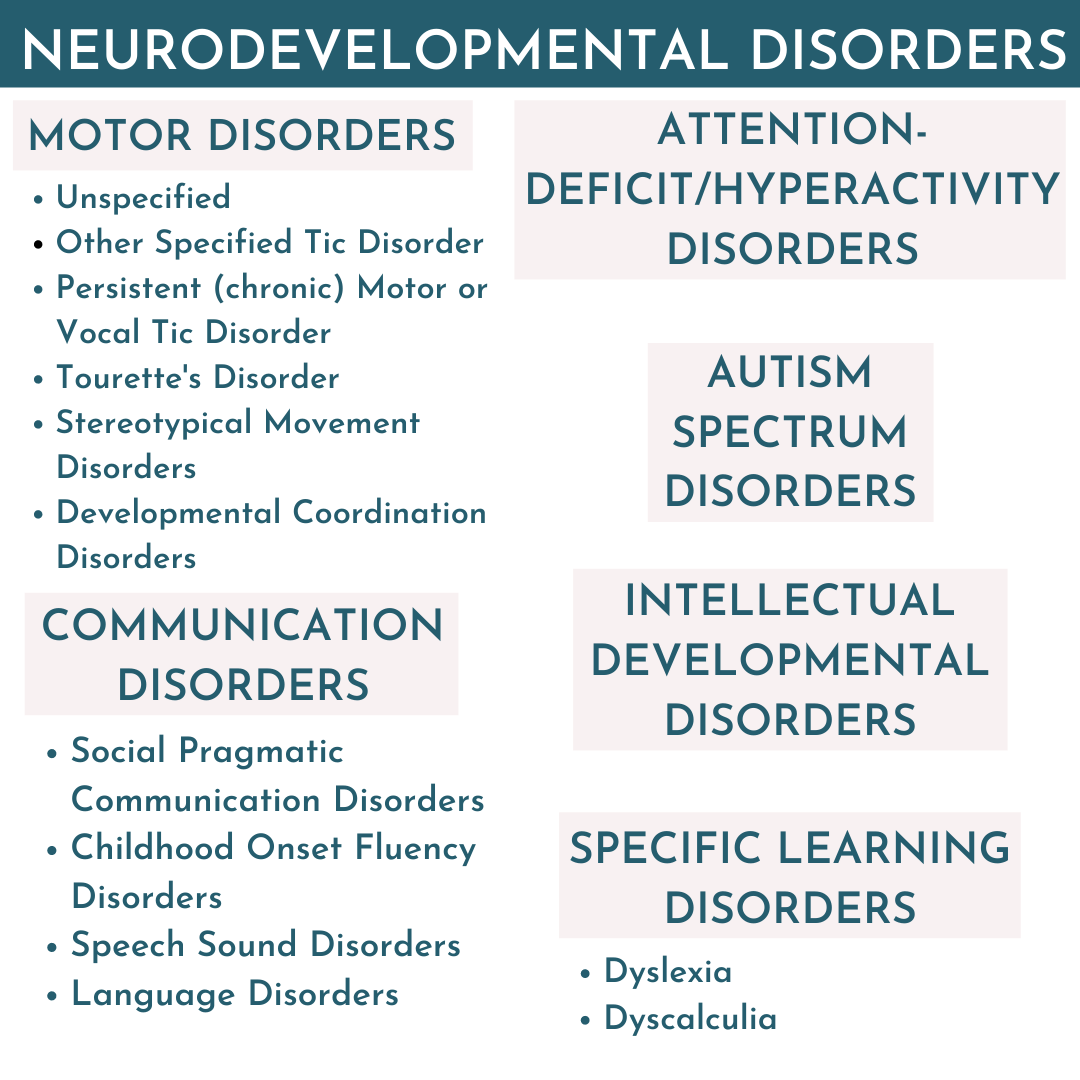
ASDs are just one type of neurodevelopmental disorder. In NDDs, the brain and nervous system are impacted during critical development periods and they’re often diagnosed before the child enters preschool. Currently, 1 in 6 American children have a diagnosed NDD [7]. These are neurological conditions where the biology of the body has direct influence of the brain (a bi-directional relationship), mood, and overall health and functioning.
Other examples of neurodevelopmental disorders on the rise in addition to ASDs (and sometimes overlapping with) include but are not limited to [8];
Attention-Deficit/Hyperactivity Disorders - 1 in 10 U.S. children diagnosed [9]
Communication Disorders
Childhood Apraxia of Speech, Speech Sound Disorders, Language Disorders, Childhood-onset Fluency Disorders, and Social (Pragmatic) Communication Disorders
Global Developmental Delay
Intellectual Developmental Disorders
Specific Learning Disorders
and more...
For so long, the mainstream thought was that ASDs and NDDs were brain-based psychological disorders, primarily caused by genetics.
While many still believe this outdated ideology, emerging literature continues to demonstrate ASDs and NDDs are biochemically influenced, all the way down to the molecular levels. [10] It is not a coincidence that the rates of ASDs have correlated with the rise of other neurodevelopmental disorders and chronic diagnoses, as many on the spectrum have underlying co-occuring NDDs and/or chronic health conditions. [11] That’s what I want the key points/“take away” from this blog to be! From my work in general. These are whole body conditions! When we address their underlying health challenges, many children experience improvements in their health and development.
Let’s pause here and spend a moment to think about this.
If a person is impacted at the molecular level, they’re impacted on the cellular level. [12] What are your tissues and organs made of? Cells! When cells are impaired, organs become impaired, systems become impaired. Whole body systems are becoming impaired!
These are whole body conditions that deserve attention accordingly! It is no longer a secret or surprise that children and individuals with ASDs have generally poorer health compared to their neurotypically matched peers. [13]
Below are some of the co-occurring conditions found to be overlapping in children and individuals with autism/ASDs:
ADHDs
Communication Disorders
Feeding Disorders
Sleep Disorders
Epilepsy / Seizures
Asthma and Respiratory
Eczema
Chronic Ear Infections
Anxiety Disorders
Obsessive Compulsive Disorder
PANS/PANDAS Conditions
Gastrointestinal Disorders
Autoimmune Conditions
Food Allergies and Intolerances [14]
Chemical Intolerances [14]
The rates of these comorbidities is certainly further evidence elucidating these conditions as whole body conditions.
Overlapping underlying commonalities these comorbid conditions above share:
Genetic Predispositions
Sensitivity to Environmental Stressors
Impaired Detoxification
Oxidative Stress
Mitochondrial Dysfunction
Poor Digestion
Dysbiosis of the Gut
Intestinal Hyper-Permeability (“leaky gut”)
Systemic Inflammation
Nutritional Deficiencies
Immune Dysfunction
What has changed?
Why are we experiencing this global explosion of childhood epidemics?
In the words of Richard Louv, “The health of children and the health of the Earth are inseparable.'' Genetics alone cannot account for the dramatic increase of chronic health epidemics across the board for children and adults. There’s no way to candy coat this, we live in an increasingly toxic world. When you’re walking through the store, most of us assume if something is on the store shelf “it’s safe”. WRONG. We live in a country that doesn’t exercise the precautionary principle [15], which implies that if there are any risks to public health or the environment it’s best to avoid and not release that product or ingredient. Instead, the U.S. has allowed thousands upon thousands of inadequately tested chemicals into our country and world.
Over the past few decades, we have over 80,000 man-made chemicals on the market today that have not been adequately tested for human and environmental safety.
I’m not trying to scare you but consider that plus the essentially infinite possibilities that these chemicals could have on each of our own unique bioindividuality! Now think about the fact that we don’t know how all of these substances interact with our biology and/or the synergistic interactions of each other! That’s only considering man-made chemicals.
That’s not accounting for our lifestyle factors, as well as the agricultural, medical, and birthing practices that have significantly changed over the course of the last 100 years. We are being impacted epigenetically - our environment, food, and lifestyle decisions impact our gene expressions and overall health. These epigenetic impacts are observed as the symptoms and conditions we see rising.
What can we do for our families and the world?
Start with what you CAN control!
Traditional therapies are important but addressing a child’s underlying health status is a key step!
We can help these children and individuals and simultaneously vote for a cleaner planet for our future generations.
Aim for small and sustainable changes that have great impacts on lowering your family’s “total load” (a.k.a body burden, allostatic load, toxic load, etc.) over time. Be mindful and intentional with your spending habits. This can improve the entire family’s health and the world around us. That’s a loaded statement - I recognize that and promise I’ll continue to elaborate across my media. I think it’s empowering to see each purchase as a vote you’re casting. For example: when I buy organic produce, I'm voting for organic farming practices and I’m consuming less agricultural chemicals. When we choose organic and/or pasture raised animal products, we are voting for better animal welfare and we’re also getting better nutrient intake from healthier animals!
While it may be more expensive in the store, studies have shown organic produce [16] and healthier animals have increased nutrient qualities! No poorly tested toxicant chemicals, lower agricultural product residues, better nutrient density, and you can choose to see these purchases as preventative healthcare! Another example, you could choose to buy unscented hygiene and household products (without “fragrance” or “perfume”) and/or make your own cleaning products from frugal options like baking soda, white vinegar, salt, and lemons.
You see where I’m going with this? It’s about our daily routines and decisions about what goes into and onto our bodies. When it comes to overhauling your child and families diet, nutrition, and lifestyle - have grace with yourself. It is a process. A marathon, not a sprint! Start with what feels manageable and where the most impact will be. For example, if your child is struggling with hyperactivity - you may consider looking at removing artificial flavors, dyes/colors, preservatives, flavor enhancers, etc. then slowly overtime move towards buying only certified organic processed foods, and so forth.
So many parents from around the world are seeing incredible progress and improvements in their children and family’s health conditions by changing their nutrition and lifestyle habits. I have seen nutrition and lifestyle create miraculous changes in children that therapies alone cannot account for.
Think on it...Do you function at your best when you’re unwell? No! We all function optimally as our healthiest selves!
When we work to address their underlying biology and health, many children with NDDs and Special Needs can experience rapid progress that then supports the therapy and educational strategies they’re working on. While I personally know children who have lost their diagnosis, nutrition and lifestyle interventions are not a miracle “cure all” but they are certainly a foundational concept that we need to collectively take into account for each of these children and individuals as we move forward.
Changing your family’s diet and lifestyle can be overwhelming, especially if you’re parenting a selective “picky” eater!
Remember, you don’t have to change everything overnight and you don’t have to do it alone!
Start small and go at your own pace! We’re building a community of like minded people across my social media pages of families who have already seen remarkable changes in their children through diet and lifestyle changes, and are sharing their experiences.
Have a look around the site, social media, and don’t hesitate to reach out if you need more 1:1 support! I’m here for you and would be honored to support you through your child and family’s health journey!
Grab Your Free Guide:
The Dos and Don’ts for Parents of Complex Picky Eaters
DSM-5 Criteria. Retrieved from: https://www.autismspeaks.org/dsm-5-criteria
Zablotsky, B., Black, L., (2017). Estimated Prevalence of Children With Diagnosed Developmental Disabilities in the United States, 2014–2016. U.S. Department of Human Health Services. Centers for Disease Control. NCHS Data Brief, National Health Interview Survey, 2014–2016. (No. 291). Retrieved from: https://www.cdc.gov/nchs/data/databriefs/db291.pdf
Baio, J., Wiggins, L., Christensen DL, et al.(2018). Prevalence of Autism Spectrum Disorder Among Children Aged 8 Years — Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2014. MMWR Surveill Summ; 67(No. SS-6):1–23. DOI: http://dx.doi.org/10.15585/mmwr.ss6706a1external icon
Hertz-Picciotto, I., & Delwiche, L., et al.(2009). The rise in autism and the role of age at diagnosis. Epidemiology (Cambridge, Mass.), 20(1), 84–90. DOI:10.1097/EDE.0b013e3181902d15
Bethell, C., Kogan, M., et al. (2011). A National and State Profile of Leading Health Problems and Health Care Quality for US Children: Key Insurance Disparities and Across-State Variations. Academic Pediatrics. 11(3), S22-S33. DOI: https://doi.org/10.1016/j.acap.2010.08.011
Blue Cross Blue Shield Report (2019, April) The Health of Millenials. Retrieved from: https://www.bcbs.com/the-health-of-america/reports/the-health-of-millennials
Boyle, C., Boulet, S., et al. (2011). Trends in the Prevalence of Developmental Disabilities in US Children, 1997–2008. Pediatrics. 127(6).1034-1042; DOI: 10.1542/peds.2010-2989
Harris, C. (2014). New classification for neurodevelopmental disorders in DSM-5. Current Opinion in Psychiatry: 27(2), 95-9; DOI: 10.1097/YCO.0000000000000042
Nisser, S., Zablotsky, B., (2015). Diagnostic Experiences of Children With
Attention-Deficit/Hyperactivity Disorder. U.S. Department of Human Health Services. Centers for Disease Control. National Health Statistics Reports. (81). Retrieved from: https://www.cdc.gov/nchs/data/nhsr/nhsr081.pdf
Randolph-Gips, M., & Srinivasan, P. (2012). Modeling autism: a systems biology approach. Journal of clinical bioinformatics, 2(1), 17. DOI:10.1186/2043-9113-2-17
Croen, L. A., Zerbo, O., Qian, Y., Massolo, M. L., Rich, S., Sidney, S., & Kripke, C. (2015). The health status of adults on the autism spectrum. Autism, 19(7), 814–823. DOI: https://doi.org/10.1177/1362361315577517
Rose, S., Niyazov, D.M., Rossignol, D.A. et al.(2018) Clinical and Molecular Characteristics of Mitochondrial Dysfunction in Autism Spectrum Disorder. Molecular Diagnosis & Therapy. 22(5), 571-593.DOI: https://doi.org/10.1007/s40291-018-0352-x
Muskens, J. B., Velders, F. P., & Staal, W. G. (2017). Medical comorbidities in children and adolescents with autism spectrum disorders and attention deficit hyperactivity disorders: a systematic review. European child & adolescent psychiatry, 26(9), 1093–1103. doi:10.1007/s00787-017-1020-0
Heilbrun, L., Palmer, R. et al (2015) Maternal Chemical and Drug Intolerances: Potential Risk Factors for Autism and Attention Deficit Hyperactivity Disorder (ADHD). The Journal of the American Board of Family Medicine, 28 (4) 461-470; DOI: 10.3122/jabfm.2015.04.140192
Martuzzi, M., Tickner, J., et al. (2003) The precautionary principle: protecting public health, the environment and the future of our children. International Journal of Epidemiology 32: 489-492. Retrieved from: http://www.euro.who.int/__data/assets/pdf_file/0003/91173/E83079.pdf
Benbrook, C., et al: (2008) New Evidence Confirms the Nutritional Superiority of Plant-Based Organic Foods. The Organic Center. State of Science Review: Nutritional Superiority of Organic Foods. Retrieved from: http://www.organiccenter.org/reportfiles/5367_Nutrient_Content_SSR_FINAL_V2.pdf
"Feel the Fear and Do It Anyways"
The blog post that almost never was…
I’ve been told countless times that I should start a blog. I’ve been writing this first blog post for 5 years. Different versions and edits exist and have existed. Many have been deleted. I’ve put a lot of unnecessary pressure about what the first blog post on my website should be. I’ve let fear dictate my inaction but today I’m busting through it!
So, this first blog post is about “feeling the fear and doing it anyways”. It’s about how my own health challenges have reshaped my life’s work as a professional working with children who have different abilities and special needs.
This blog may cause you to view neurodevelopmental disorders differently. On behalf of all my amazing little friends I work with and their families, I hope that it will.
Okay so, where do I even start?
Well first, some exciting news and a little background: in January 2019, I graduated as a Nutritional Therapy Practitioner through the Nutritional Therapy Association! Graduating from the NTA is an endeavor I have desperately wanted to complete since 2014. All accomplishments are to be celebrated but I feel an overwhelming sense of gratitude as I continue to integrate my work as a holistic bio-individual nutrition professional serving this under-represented population.
Something you may or may not know about me, in the fall of 2013, I developed a chronic illness while earning my Masters of Speech-Language Pathology. It turns out, illness doesn't wait around for the perfect timing and it doesn’t discriminate. This post isn't to gather anyone's sympathy about my situation or what’s happened to me, so please, don't feel bad for me for a moment. It's not about that. I’m sharing because my own health and wellness journey has been one of the most impactful turning points in my life and career. It was the catalyst that ultimately led me to becoming an NTP and building Speaking of Health & Wellness, LLC to serve my clients in a way that combines my passions and knowledge. In hindsight, I am endlessly thankful.
I came across a card recently that I wrote myself years ago and it sparked a variety of emotions within me…
During the last academic semester, December 2014, my cohort was about to head off on holiday. One of my very passionate professors was running late for class and having a particularly rough day. She found herself caught in a back and forth with an editor or publisher (I can’t exactly recall) about a major piece of her life’s work. Her legacy that she had poured her heart and soul into, and they wanted to tailor it beyond what felt still authentically hers.
Rather than diving straight into the material, she passed out notecards for the room, instructing us to date them. She shared the details of the day she was having and continued she’d been experiencing health challenges (but was going to be alright), and apologized for the length of time it was taking her to get certain grades back to us. The room was quiet. Many of us were shocked that she was sharing so personally in this way. She didn’t intend to make us feel sorry for her though. It was meant to be a moment of truth and realness. Likely to be judged but she didn’t care. She “felt the fear and did it anyways”. In her frazzle and honesty, she was so vulnerably human and inspiring to me, especially in the midst of what I was going through in my own health journey.
She put the class material on pause to share her own rawness with us and inspire us to be creators of change in our lives and careers. She spoke about passion and leaving a legacy. She challenged us to check in with ourselves as we concluded our final week of SLP Masters coursework, and think about the work and purpose that we would give to the world…and then write it onto the card. Put it out there. As you may have expected, she gave us heads up that if we were comfortable we should share them aloud in class as colleagues, and then keep them for ourselves to reflect on.
I was terrified to share my truth
but I wanted to take the moment and opportunity seriously
At that time, I was slightly over a year into my health journey. I was under the care of a Naturopathic Doctor and her Registered Nurse/Nutritional Therapist after visiting numerous allopathic doctors without answers or relief. I was improving my health and lifestyle rapidly to keep up with my food and environmental sensitivities. I was fatigued, battling chronic pain, and experiencing a body burden overload.
Meanwhile, I was learning a number of highly inconvenient truths about our food, healthcare, educational systems and industries, along with our government agencies. In my learning I came across financial ties and a series of issues that made me uncomfortable and more cautious with my purchases. I was upset about my circumstances and grieving in many ways, but desperately determined to create something positive from my circumstances. I can see that so clearly now when I look at the language I used on my card below…
When you read it, if I seem angry, it’s because I was.
And for the record, I no longer refer to myself as someone who is “sick”. Our word choices influence our mindset and thoughts, which influence our reality. I now choose “healing” and try to be mindful of the way I speak of my health.
The Naturopathic Doctor and Registered Nurse/Nutritional Therapist that I was seeing had both strongly encouraged me to look into autism spectrum disorders as whole body conditions when they learned what I was studying. This stretched my mental capacity in many ways to consider and learn about but since then I’ve been consumed with the topic.
As it turns out, there is a plethora of literature that currently exists and their publications are not slowing any time soon. An increasing body of evidence exists to support that autism spectrum disorders (at least certain subgroups of) are whole body epigenetic conditions. [1.] The challenge is getting this literature in the hands of the public and professionals to be accepted as mainstream knowledge in the face of an estimated 17 year research lag! [2.]
On 12/1/14 - As everyone took their turns reading their cards aloud, I realized I’d probably be sharing. After all, I didn’t want to be the only one who didn’t share, right? Feeling nervous but inspired by my professor, I divulged my own health challenges on my card and proclaimed that I was going to become a Nutritional Therapy Practitioner to integrate my knowledge as an SLP and feeding specialist to work with children and families impacted by autism and other neurodevelopmental disorders we serve as SLPs. I assumed that for most of my classmates this idea probably sounded like a foreign concept. I recognize that this may even feel like a far out concept for readers of this blog today! If this applies to you, thank you for taking the time and having the open mindedness to read and learn.
One thing was certain that day:
I knew even before I graduated as an SLP that I had to somehow incorporate a way of sharing what I had been learning about holistic nutrition and lifestyle impacts on our health into my career. Specifically, I knew I wanted to work with children and families with neurodevelopmental disorders, combining my passions for holistic development, parent coaching, and my love for nutrition.
I’ve learned and recognized that generally all children with neurodevelopmental disorders (i.e. ASDs, ADHDs, SPDs, apraxia, dyslexia, etc.) and special needs (i.e. Down syndrome, chromosomal differences, etc.) can likely benefit from diet, nutrition, and lifestyle strategies in varying capacities. These benefits often include the improved reception and faster generalization of concepts and skills being taught in traditional therapies, like speech-language, occupational, physical, and behavioral therapies!
This was my truth but I was terrified of what my classmates would think. What would my professor think? So much fear of the judgment of others, even though I knew I had established and emerging research supporting what I was sharing. When my turn came, I “felt the fear and did it anyways”. I did not read the card verbatim, as you can see there’s a lot of emotion behind it, but I shared it. I shared that children could be helped in an integrative way through nutrition and lifestyle, and my mission to become an NTP publicly and aloud to my classmates.
And you know what? The world kept spinning!
Not only did it keep spinning but my world has continued to perfectly align to make it all happen since that time. Now here I am: I’ve become an NTP and Documenting Hope Certified Health Coach, and the proud business owner of my life’s work, Speaking of Health & Wellness, LLC. I’m not saying that everything just fell into place! Believe me, I’ve put in the work to grow into the person and professional I am. The concepts of courage and self-growth take a new level of meaning when you’re an individual managing a chronic condition, dedicated to being a life long student, stepping further into entrepreneurship, all while trying your best in your personal life.
I shared the card and the world kept spinning, and years later I turned the card into reality! I felt a sense of pride and joy for myself when I found this card and it gave me some extra motivation to start writing. And here I am sharing my first blog post on a blog that I’d been nervous to start…
The blog post that almost never was
and I am certain the world will keep spinning
I’m “feeling the fear and doing it anyways”
One of my favorite aspects of becoming a speech-language pathologist was the concept of literally helping give a voice to the voice-less, via whatever we needed to do for that individual’s best communication and quality of life.
My vision is that Speaking of Health & Wellness will be a voice for the voice-less on a massive wide-spread scale, beyond just the clients I am able to work with one-on-one.
I envision a global community and network. I aim to advocate on behalf of these children and their families, spreading the awareness that they can be helped in more impactful and integrative ways. Holistic nutrition and low-toxicant living can profoundly impact children’s health, wellness, and development.
It is my sincere hope the contents of this site moving forward will serve as a starting point for families everywhere!
I hope that by visiting this site and following along on social media, you are reminded to
speak your truth
I hope that my story will inspire you to
follow your heart and your purpose
& I hope that you’ll be encouraged to
“feel the fear and do it anyways”
To you and your family’s health!
Shandy
“Everything you’ve ever wanted is sitting on the other side of fear”
– George Addair
Stayed tuned for more posts to come!
CLICK BELOW to join our FREE Facebook Community!
1. Randolph-Gips, M., & Srinivasan, P. (2012). Modeling autism: a systems biology approach. Journal of clinical bioinformatics, 2(1), 17. doi:10.1186/2043-9113-2-17
2. Morris, Z. S., Wooding, S., & Grant, J. (2011). The answer is 17 years, what is the question: understanding time lags in translational research. Journal of the Royal Society of Medicine, 104(12), 510–520. https://doi.org/10.1258/jrsm.2011.110180