Exploring Autism & Other Neurodevelopmental Disorders as Whole Body Conditions [Blog]
[Click here to listen to my accompanying podcast, “Exploring Autism & Other Neurodevelopmental Disorders as Whole Body Conditions”]
I will continue to build on this topic but for now (before I get too ahead of myself), let’s get into some foundational information about autism spectrum disorders & other neurodevelopmental disorders as whole body conditions.
I hope that this blog will be a good starting point to help evolve your perception of autism spectrum disorders (ASDs) and neurodevelopmental disorders (NDDs) in general.
ASDs are referred to as “spectrum” disorders to reflect the vast varieties of skills and symptoms of each individual, while also sharing similarities. Most autism researchers agree that we are beginning to be able to recognize different subtype groups of individuals on the spectrum, based on causes, treatments, and related commonalities.
There’s a quote in the world of autism, “If you’ve met one person with autism, you’ve met one person with autism” by Dr. Stephen Shore. Meaning, don’t think that you know what “autism looks like” because you’ve met one or a few children or individuals on the spectrum. I have personally worked with children on the spectrum for a decade and fully agree with this quote in a number of ways.
Since you’re here, you probably already know the common symptoms and signs of ASDs but just in case you don’t, let’s review them briefly.
According to the DSM-5 [1], the diagnostic criteria for ASDs are based upon symptoms/traits that include:
“Persistent deficits in social communication and social interaction across multiple contexts”
“Restricted, repetitive patterns of behavior, interests, or activities.”
“Symptoms cause clinically significant impairment in social, occupational, or other important areas of current functioning.”
For perspective, in the 70s / early 80s, it was said to be at 1 in 10,000 children. According to CDC data, autism spectrum disorders now impact 1 in 36 children [2]...or 1 in 59 [3] depending on which CDC data you chose... That’s a separate blog for a later time.
The point is that we’re at epidemic rates. Rates that are unsustainable for families, our nation, and the world if we are to truly help support these children/individuals and their families obtain the resources and supports they need access to!
Some argue that the rise in diagnosis can be attributed to better diagnosis, earlier diagnosis, and changes in diagnostic criteria. I find this implication oversimplified and relatively dismissive. As a pediatric SLP, I’ll be the first to admit I have witnessed some over diagnosis but the reality is that a change in or increased identification of ASDs cannot account for even half of the increased rates we’ve seen over time. Not only across our country but also around the world.
Per Hertz-Picciotto in a 2009 study published in Epidemiology, earlier diagnosis and changes in diagnostic criteria only accounted for ~1/3 of the increase in total rates of ASD [4].
When I am faced with the “it’s better diagnosis” response, I like to bring the conversation to the bigger picture. The rates of chronic illness in children and adults have increased significantly in the last 2-3 decades. Over half, (~54%) of both children [5] and millenials [6] have a diagnosed chronic health condition. With this information we can reflectively say that society at large is experiencing a health crisis.
ASDs are just one type of neurodevelopmental disorder. In NDDs, the brain and nervous system are impacted during critical development periods and they’re often diagnosed before the child enters preschool. Currently, 1 in 6 American children have a diagnosed NDD [7]. These are neurological conditions where the biology of the body has direct influence of the brain (a bi-directional relationship), mood, and overall health and functioning.
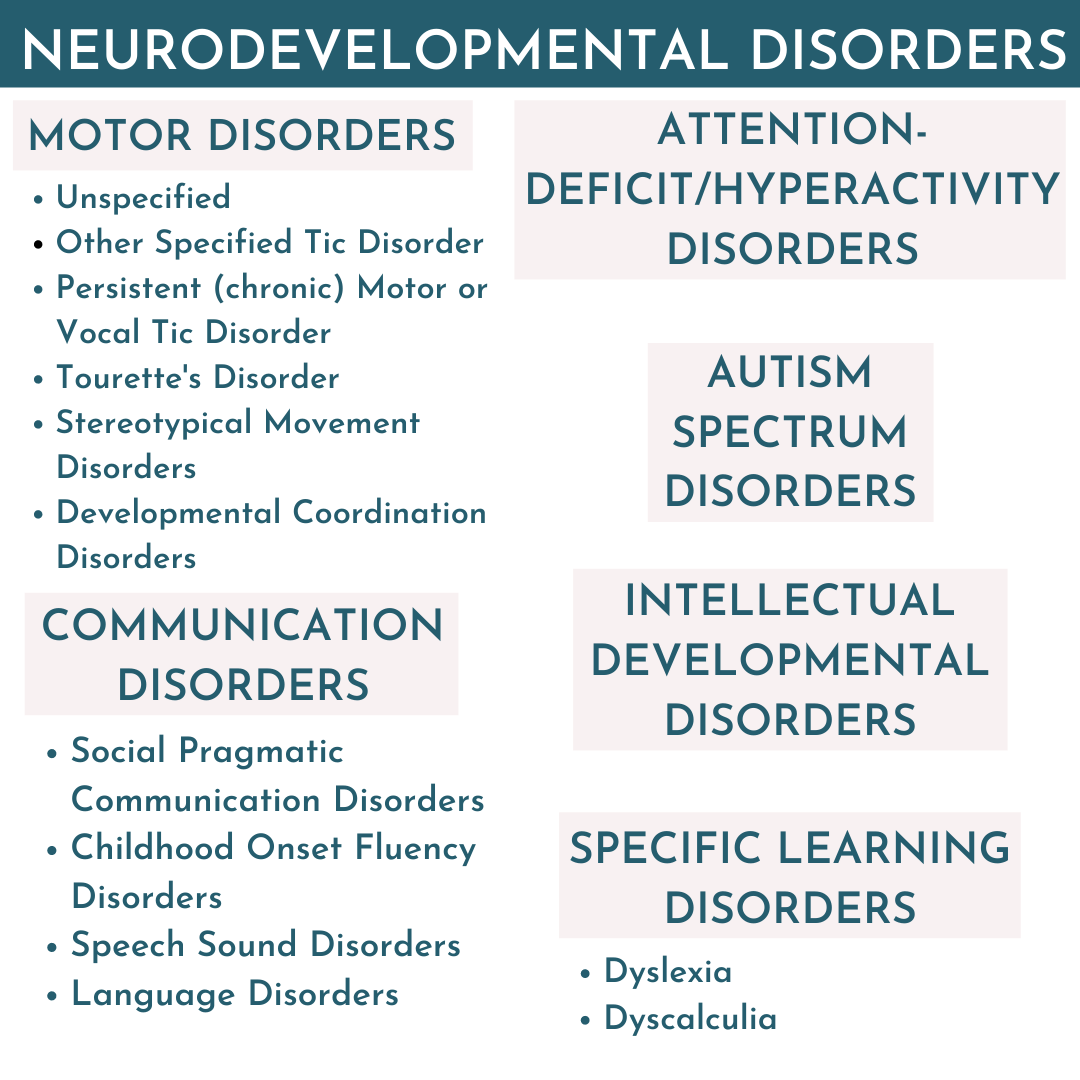
Other examples of neurodevelopmental disorders on the rise in addition to ASDs (and sometimes overlapping with) include but are not limited to [8];
Attention-Deficit/Hyperactivity Disorders - 1 in 10 U.S. children diagnosed [9]
Communication Disorders
Childhood Apraxia of Speech, Speech Sound Disorders, Language Disorders, Childhood-onset Fluency Disorders, and Social (Pragmatic) Communication Disorders
Global Developmental Delay
Intellectual Developmental Disorders
Specific Learning Disorders
and more...
For so long, the mainstream thought was that ASDs and NDDs were brain-based psychological disorders, primarily caused by genetics.
While many still believe this outdated ideology, emerging literature continues to demonstrate ASDs and NDDs are biochemically influenced, all the way down to the molecular levels. [10] It is not a coincidence that the rates of ASDs have correlated with the rise of other neurodevelopmental disorders and chronic diagnoses, as many on the spectrum have underlying co-occuring NDDs and/or chronic health conditions. [11] That’s what I want the key points/“take away” from this blog to be! From my work in general. These are whole body conditions! When we address their underlying health challenges, many children experience improvements in their health and development.
Let’s pause here and spend a moment to think about this.
If a person is impacted at the molecular level, they’re impacted on the cellular level. [12] What are your tissues and organs made of? Cells! When cells are impaired, organs become impaired, systems become impaired. Whole body systems are becoming impaired!
These are whole body conditions that deserve attention accordingly! It is no longer a secret or surprise that children and individuals with ASDs have generally poorer health compared to their neurotypically matched peers. [13]
Below are some of the co-occurring conditions found to be overlapping in children and individuals with autism/ASDs:
ADHDs
Communication Disorders
Feeding Disorders
Sleep Disorders
Epilepsy / Seizures
Asthma and Respiratory
Eczema
Chronic Ear Infections
Anxiety Disorders
Obsessive Compulsive Disorder
PANS/PANDAS Conditions
Gastrointestinal Disorders
Autoimmune Conditions
Food Allergies and Intolerances [14]
Chemical Intolerances [14]
The rates of these comorbidities is certainly further evidence elucidating these conditions as whole body conditions.
Overlapping underlying commonalities these comorbid conditions above share:
Genetic Predispositions
Sensitivity to Environmental Stressors
Impaired Detoxification
Oxidative Stress
Mitochondrial Dysfunction
Poor Digestion
Dysbiosis of the Gut
Intestinal Hyper-Permeability (“leaky gut”)
Systemic Inflammation
Nutritional Deficiencies
Immune Dysfunction
What has changed?
Why are we experiencing this global explosion of childhood epidemics?
In the words of Richard Louv, “The health of children and the health of the Earth are inseparable.'' Genetics alone cannot account for the dramatic increase of chronic health epidemics across the board for children and adults. There’s no way to candy coat this, we live in an increasingly toxic world. When you’re walking through the store, most of us assume if something is on the store shelf “it’s safe”. WRONG. We live in a country that doesn’t exercise the precautionary principle [15], which implies that if there are any risks to public health or the environment it’s best to avoid and not release that product or ingredient. Instead, the U.S. has allowed thousands upon thousands of inadequately tested chemicals into our country and world.
Over the past few decades, we have over 80,000 man-made chemicals on the market today that have not been adequately tested for human and environmental safety.
I’m not trying to scare you but consider that plus the essentially infinite possibilities that these chemicals could have on each of our own unique bioindividuality! Now think about the fact that we don’t know how all of these substances interact with our biology and/or the synergistic interactions of each other! That’s only considering man-made chemicals.
That’s not accounting for our lifestyle factors, as well as the agricultural, medical, and birthing practices that have significantly changed over the course of the last 100 years. We are being impacted epigenetically - our environment, food, and lifestyle decisions impact our gene expressions and overall health. These epigenetic impacts are observed as the symptoms and conditions we see rising.
What can we do for our families and the world?
Start with what you CAN control!
Traditional therapies are important but addressing a child’s underlying health status is a key step!
We can help these children and individuals and simultaneously vote for a cleaner planet for our future generations.
Aim for small and sustainable changes that have great impacts on lowering your family’s “total load” (a.k.a body burden, allostatic load, toxic load, etc.) over time. Be mindful and intentional with your spending habits. This can improve the entire family’s health and the world around us. That’s a loaded statement - I recognize that and promise I’ll continue to elaborate across my media. I think it’s empowering to see each purchase as a vote you’re casting. For example: when I buy organic produce, I'm voting for organic farming practices and I’m consuming less agricultural chemicals. When we choose organic and/or pasture raised animal products, we are voting for better animal welfare and we’re also getting better nutrient intake from healthier animals!
While it may be more expensive in the store, studies have shown organic produce [16] and healthier animals have increased nutrient qualities! No poorly tested toxicant chemicals, lower agricultural product residues, better nutrient density, and you can choose to see these purchases as preventative healthcare! Another example, you could choose to buy unscented hygiene and household products (without “fragrance” or “perfume”) and/or make your own cleaning products from frugal options like baking soda, white vinegar, salt, and lemons.
You see where I’m going with this? It’s about our daily routines and decisions about what goes into and onto our bodies. When it comes to overhauling your child and families diet, nutrition, and lifestyle - have grace with yourself. It is a process. A marathon, not a sprint! Start with what feels manageable and where the most impact will be. For example, if your child is struggling with hyperactivity - you may consider looking at removing artificial flavors, dyes/colors, preservatives, flavor enhancers, etc. then slowly overtime move towards buying only certified organic processed foods, and so forth.
So many parents from around the world are seeing incredible progress and improvements in their children and family’s health conditions by changing their nutrition and lifestyle habits. I have seen nutrition and lifestyle create miraculous changes in children that therapies alone cannot account for.
Think on it...Do you function at your best when you’re unwell? No! We all function optimally as our healthiest selves!
When we work to address their underlying biology and health, many children with NDDs and Special Needs can experience rapid progress that then supports the therapy and educational strategies they’re working on. While I personally know children who have lost their diagnosis, nutrition and lifestyle interventions are not a miracle “cure all” but they are certainly a foundational concept that we need to collectively take into account for each of these children and individuals as we move forward.
Changing your family’s diet and lifestyle can be overwhelming, especially if you’re parenting a selective “picky” eater!
Remember, you don’t have to change everything overnight and you don’t have to do it alone!
Start small and go at your own pace! We’re building a community of like minded people across my social media pages of families who have already seen remarkable changes in their children through diet and lifestyle changes, and are sharing their experiences.
Have a look around the site, social media, and don’t hesitate to reach out if you need more 1:1 support! I’m here for you and would be honored to support you through your child and family’s health journey!
Grab Your Free Guide:
The Dos and Don’ts for Parents of Complex Picky Eaters
DSM-5 Criteria. Retrieved from: https://www.autismspeaks.org/dsm-5-criteria
Zablotsky, B., Black, L., (2017). Estimated Prevalence of Children With Diagnosed Developmental Disabilities in the United States, 2014–2016. U.S. Department of Human Health Services. Centers for Disease Control. NCHS Data Brief, National Health Interview Survey, 2014–2016. (No. 291). Retrieved from: https://www.cdc.gov/nchs/data/databriefs/db291.pdf
Baio, J., Wiggins, L., Christensen DL, et al.(2018). Prevalence of Autism Spectrum Disorder Among Children Aged 8 Years — Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2014. MMWR Surveill Summ; 67(No. SS-6):1–23. DOI: http://dx.doi.org/10.15585/mmwr.ss6706a1external icon
Hertz-Picciotto, I., & Delwiche, L., et al.(2009). The rise in autism and the role of age at diagnosis. Epidemiology (Cambridge, Mass.), 20(1), 84–90. DOI:10.1097/EDE.0b013e3181902d15
Bethell, C., Kogan, M., et al. (2011). A National and State Profile of Leading Health Problems and Health Care Quality for US Children: Key Insurance Disparities and Across-State Variations. Academic Pediatrics. 11(3), S22-S33. DOI: https://doi.org/10.1016/j.acap.2010.08.011
Blue Cross Blue Shield Report (2019, April) The Health of Millenials. Retrieved from: https://www.bcbs.com/the-health-of-america/reports/the-health-of-millennials
Boyle, C., Boulet, S., et al. (2011). Trends in the Prevalence of Developmental Disabilities in US Children, 1997–2008. Pediatrics. 127(6).1034-1042; DOI: 10.1542/peds.2010-2989
Harris, C. (2014). New classification for neurodevelopmental disorders in DSM-5. Current Opinion in Psychiatry: 27(2), 95-9; DOI: 10.1097/YCO.0000000000000042
Nisser, S., Zablotsky, B., (2015). Diagnostic Experiences of Children With
Attention-Deficit/Hyperactivity Disorder. U.S. Department of Human Health Services. Centers for Disease Control. National Health Statistics Reports. (81). Retrieved from: https://www.cdc.gov/nchs/data/nhsr/nhsr081.pdf
Randolph-Gips, M., & Srinivasan, P. (2012). Modeling autism: a systems biology approach. Journal of clinical bioinformatics, 2(1), 17. DOI:10.1186/2043-9113-2-17
Croen, L. A., Zerbo, O., Qian, Y., Massolo, M. L., Rich, S., Sidney, S., & Kripke, C. (2015). The health status of adults on the autism spectrum. Autism, 19(7), 814–823. DOI: https://doi.org/10.1177/1362361315577517
Rose, S., Niyazov, D.M., Rossignol, D.A. et al.(2018) Clinical and Molecular Characteristics of Mitochondrial Dysfunction in Autism Spectrum Disorder. Molecular Diagnosis & Therapy. 22(5), 571-593.DOI: https://doi.org/10.1007/s40291-018-0352-x
Muskens, J. B., Velders, F. P., & Staal, W. G. (2017). Medical comorbidities in children and adolescents with autism spectrum disorders and attention deficit hyperactivity disorders: a systematic review. European child & adolescent psychiatry, 26(9), 1093–1103. doi:10.1007/s00787-017-1020-0
Heilbrun, L., Palmer, R. et al (2015) Maternal Chemical and Drug Intolerances: Potential Risk Factors for Autism and Attention Deficit Hyperactivity Disorder (ADHD). The Journal of the American Board of Family Medicine, 28 (4) 461-470; DOI: 10.3122/jabfm.2015.04.140192
Martuzzi, M., Tickner, J., et al. (2003) The precautionary principle: protecting public health, the environment and the future of our children. International Journal of Epidemiology 32: 489-492. Retrieved from: http://www.euro.who.int/__data/assets/pdf_file/0003/91173/E83079.pdf
Benbrook, C., et al: (2008) New Evidence Confirms the Nutritional Superiority of Plant-Based Organic Foods. The Organic Center. State of Science Review: Nutritional Superiority of Organic Foods. Retrieved from: http://www.organiccenter.org/reportfiles/5367_Nutrient_Content_SSR_FINAL_V2.pdf